
March 17th, 2022 - Press notes
Study published in Nature Cancer
Researchers at the Hospital del Mar Medical Research Institute and Hospital del Mar have transformed immunotherapy-resistant tumours into tumours that respond to this treatment, achieving cures in animal models through an innovative therapeutic strategy in triple-negative breast cancer, the most aggressive subtype. Researchers have discovered the essential role of a new factor, LCOR, in enabling cancer cells to present tumour antigens on their surfaces. These antigens allow the immune system to recognise the tumour, an essential step if immunotherapy treatment is to succeed. On the other hand, they have shown that cancer stem cells have very low levels of LCOR, making them invisible to the immune system and therefore resistant to treatment.
The work that has just been published used an innovative experimental messenger RNA system, similar to the technology used for COVID-19 vaccines, to produce LCOR in tumour cells. In this way, the resistant tumour cells of triple-negative cancer become visible and sensitive to the immune system. This approach is also being investigated in other breast cancer subtypes. Currently, the clinical use of immunotherapy in breast cancer is limited to the triple-negative subtype. The results have been positive, but far from the level of success achieved in other tumours. This publication now opens up a new avenue for the development of therapeutic strategies to restore LCOR in immunotherapy-resistant cells that can be applied in clinical trials, thereby significantly improving immunotherapy effectiveness.
A study published in the journal Nature Cancer, carried out within the Cancer Programme at the Hospital del Mar Medical Research Institute (IMIM-Hospital del Mar) by the Cancer Stem Cells and Metastasis Dynamics Laboratory, led by Dr. Toni Celià-Terrassa, and the Laboratory of Molecular Cancer Therapy, coordinated by Dr. Joan Albanell, with the participation of international centres, has discovered an approach that radically increases the success of immunotherapy in one of the most aggressive types of tumours, triple-negative breast cancer. This subtype, although accounting for only 15% of cases, is one of the most rapidly progressing and affects younger patients. In this work, researchers found that tumour stem cells are the main cause of immunotherapy resistance in this subtype of breast cancer. The reason is that these cells are invisible to the immune system, making immunotherapy ineffective. In addition, the study offers a promising solution to this situation by using a new therapeutic approach in preclinical models that makes cancer stem cells visible to the immune system so that it can then eliminate the tumour.
Left to right, Joan Albanell, Toni Celià-Terrassa, Iván Pérez-Núñez
This subpopulation of more aggressive cells may represent between 5% and 50% of the entire tumour population in triple-negative breast cancer. They have low levels of LCOR factor, which plays a key but previously unknown role in allowing cells to present antigens on their surface, molecules that enable the immune system to differentiate normal cells from tumour cells and attack the latter. Consequently, in the case of tumour stem cells, the low presence of this LCOR factor makes them invisible to the body's defences. As a result, these cells are resistant to breast cancer immunotherapy, which has a relatively low success rate in current clinical practice.
This ability of tumour stem cells to remain invisible to the immune system allows them to withstand immunotherapy treatment. As Dr. Toni Celià-Terrassa explains, "We have seen how, despite immunotherapy treatment, these cells survive and have the ability to generate resistance, which is linked to their ability to hide from the immune system, allowing them to evade immunotherapy."
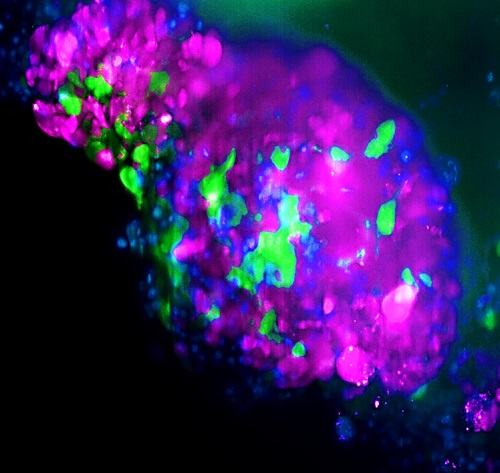
Detail of an organoid where the green cells are stem cancer cells, which do not express LCOR
Using mouse models, the researchers have demonstrated how this situation is reversed when the LCOR gene is activated in this type of cell, setting in motion the machinery that allows the immune system to detect the tumour. "It involves reconfiguring the tumour to make it completely visible and, therefore, sensitive to immunotherapy, transforming it from invisible to visible", says Iván Pérez-Núñez, a pre-doctoral researcher in the Cancer Stem Cells and Metastasis Dynamics Laboratory and first author of the study. The researchers were able to see how, by combining this approach with immunotherapy, the treatment response rate was total, and all tumours were eliminated, curing the mice in the long term. This prevents both the recurrence of cancer and the generation of resistance.
Inspired by the technology used in the design of messenger-RNA vaccines for COVID-19, the researchers decided to use a similar strategy to transport and deliver LCOR gene RNA into tumour cells and trigger its function. Biological nanovesicles, small bag-like structures formed in the cells, were developed to carry this information and were shown to do so successfully, preventing the tumour stem cells from remaining invisible.
"What we are doing is making the immune system see the tumour cell better. Unlike healthy cells, malignant cells have a much higher load of recognised 'foreign' antigens, which are not inherent to the immune system. In this way, the body's natural defences will recognise, attack and eliminate the malignant cells", explains Dr. Celià-Terrassa. In this sense, he points out that "We have discovered how to make this type of breast cancer respond to immunotherapy in preclinical models, making these cells visible thanks to the use of the antigen-presenting mechanism, thereby boosting the immunotherapy response and its efficiency."
This strategy may be applicable to other types of breast cancer tumours and other tumour types, although safety studies and clinical trials in humans are needed first. Even so, according to Dr. Joan Albanell, co-leader of the study, director of the Cancer Research Programme at IMIM-Hospital del Mar and head of the Oncology Department at Hospital del Mar, this approach does open up new possibilities. "What is important is that the experimental results demonstrate an unprecedented sensitisation of triple-negative breast cancer to immunotherapy, making resistant tumours virtually curable", says Dr Albanell, also a professor at the Universitat Pompeu Fabra. "This unequivocally motivates us to investigate therapeutic strategies that may culminate in clinical trials, and to explore whether it could be applicable to other tumours", he concludes.
The use of LCOR in combination with immunotherapy has generated a patent and a spin-off company will be created to develop this. "The project led by Dr. Celià-Terrassa and Dr. Albanell is a paradigmatic example of research in immune therapies that will be boosted in the near future by the new Immuno-oncology Division that we are creating at the IMIM", explains Dr. Joaquín Arribas, director of the IMIM-Hospital del Mar and author of the study.
The study was made possible thanks to a CLIP grant from the US Cancer Research Institute and funding from the Carlos III Health Institute (ISCIII). Thanks also go to the Spanish Association Against Cancer (Asociación Española contra el Cáncer), the Fero Foundation and CIBERONC, a centre to which the two researchers who led the study also belong.
Immunotherapy is one of the most promising treatments for eradicating tumours and curing cancer. Unfortunately, for breast cancers it is only approved in the triple-negative breast cancer subtype, where the outcomes are still far from what is expected from immunotherapy. Making immunotherapy work in breast cancer would be a great therapeutic opportunity for the breast cancer population, making it a very good option for more advanced and metastatic cases. It should be remembered that metastatic breast cancer, despite significant and continuous advances, is still not curable in the majority of patients.
At Hospital del Mar, cancer is addressed through the diagnostic tools necessary to achieve a precision diagnosis that makes it possible to plan and offer patients personalised and individualised therapeutic options according to their particular circumstances. At the same time, there is a commitment to a patient-centred care model through pioneering and benchmark work in multidisciplinary functional units specific to each type of tumour. The units, comprising professionals specialising in each cancer type, offer the best therapeutic options in a model of shared decision-making with the patient. Nurse managers guide patients through the diagnostic and therapeutic process. This quality care is combined with groundbreaking cancer research at the Hospital del Mar Medical Research Institute (IMIM) and an extensive programme of clinical trials. The research areas focus on furthering immunotherapy and liquid biopsy, searching for biomarkers and new therapeutic targets, and developing new surgery and radiotherapy strategies to improve efficacy and the quality of life of patients. This research generates almost 200 articles in scientific publications each year, two out of three of which are in high-impact journals. This state-of-the-art care and research are the basis for teaching excellence at the Hospital del Mar Campus.
Pérez-Núñez I, Rozalén C, Palomeque JA, Sangrador I, Dalmau M, Comerma L, Hernández-Prat A, Casadevall D, Menendez S, Liu DD, Shen M, Berenguer J, Rius Ruiz I, Peña R, Montañés JC, Albà MM, Bonnin S, Ponomarenko J, Gomis RR, Cejalvo JM, Servitja S, Marzese DM, Morey Ll, Voorwerk L, Arribas J, Bermejo B, Kok M, Pusztai L, Kang Y, Albanell J, Celià-Terrassa T. LCOR mediates interferon-independent tumor immunogenicity and responsiveness to immune-checkpoint blockade in triple negative breast cancer. Nature Cancer (2022) https://www.nature.com/articles/s43018-022-00339-4
Parc Salut Mar
Passeig Marítim 25-29 Barcelona 08003
See location on Google maps
Phone: 93 248 30 00 · Fax: 93 248 32 54
Information request
© 2006 - 2025 Hospital del Mar · Legal notice and Privacy Police | Cookie Policy | Accessibility